Study Reveals Promising Approach: Boosting Beta Cells to Treat Type 2 Diabetes
Researchers at Weill Cornell Medicine have uncovered a novel route to stimulate the growth of healthy insulin-producing pancreatic beta cells in a preclinical model of diabetes. The findings hold promise for future therapeutics that will improve the lives of individuals with Type 2 diabetes – a condition that affects more than 500 million people worldwide.
The study, published Sept. 15 in the Journal of Clinical Investigation, demonstrated that activating a pathway to promote cell division not only expanded the population of insulin-producing cells, but also enhanced the cells’ function.
“That’s reassuring because there is a long-standing belief in the field that proliferation can lead to ‘de-differentiation’ and a loss of cell function,” said study senior author Dr. Laura Alonso, chief of the division of endocrinology, diabetes and metabolism, director of the Weill Center for Metabolic Health and the E. Hugh Luckey Distinguished Professor in Medicine at Weill Cornell Medicine. “Our result flies in the face of that dogma and suggests if we can find a way to trigger replication of the beta cells in the body, we won’t impair their ability to produce and secrete insulin.”
First author Rachel Stamateris also contributed to this work as an M.D./Ph.D. student at the University of Massachusetts Medical School and visiting graduate assistant in medicine at Weill Cornell Medicine.
In Type 2 diabetes, which is typically associated with obesity, the body’s tissues become resistant to insulin, which means they can’t take in and use blood sugar. At the same time, insulin-producing beta cells in the pancreas fail – diminishing in number and losing their ability to function.
Alonso and her colleagues reproduced these conditions in a mouse model of diabetes that lacks IRS2, a protein that allows insulin to transmit its signal for cells to absorb blood sugar. These mice displayed insulin resistance, a seminal feature of human Type 2 diabetes. “On top of that,” Alonso said, “the IRS2 protein also turns out to be critical for beta cell function and beta cell number.”
With their pool of beta cells depleted, the first order of business to rescue these mice was to boost beta cell numbers. But how? She and her team took a closer look at the molecular machinery that controls cell proliferation. The researchers observed that in the IRS-deficient diabetic mice, beta cells failed to elevate production of cyclin D2. This protein, when partnered with a protein called CDK4, drives cell division. Previous studies had shown that mice lacking CDK4 also develop diabetes.
It seemed logical to test if boosting CDK4 activity would help increase beta cell quantity.
When Alonso’s team genetically introduced an active form of CDK4 into the diabetic mice that was more available to attach to cyclin D2, the first thing they noticed was the animals’ blood sugars were restored to normal. Their beta cells were more plentiful than in the untreated, IRS2 mutant mice.
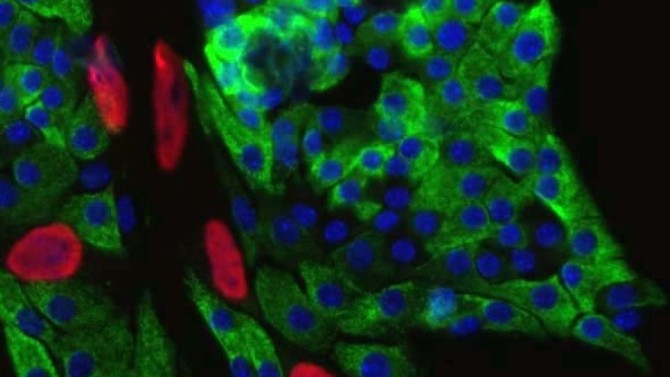
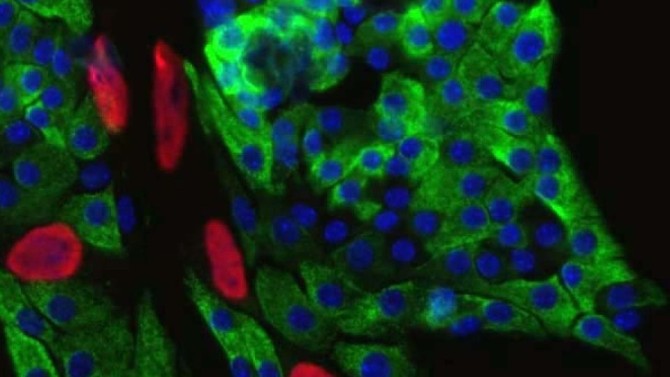
But even better: “The beta cells looked amazingly healthy in the treated mice compared with the original diabetic mice, whose beta cells look terrible. Increasing the activity of CDK4 resulted in beta cells packed full of insulin,” said Alonso, who is also an endocrinologist at NewYork-Presbyterian/Weill Cornell Medical Center.
This supports the concept that beta cell mass can be expanded without compromising function.
While CDK4 is not, itself, a viable therapeutic target because its ability to stimulate proliferation could increase the risk of cancer, Alonso is confident that probing the molecular pathways that govern beta cell division and function could someday lead to a clinical breakthrough. She pointed to Ozempic, one of the most talked-about new treatments for diabetes.
“That medication was discovered by a scientist studying toxins in the saliva of the Gila monster,” Alonso said. “So, it’s clear that understanding how fundamental biology works can lead to real advances in treating or even preventing diabetes.”
This work was supported by grants from the National Institute of Diabetes and Digestive and Kidney Diseases.