Dalhousie University Scientists Pioneer Device Enhancing Spinal Surgery Success
It’s estimated that 80 per cent of people will experience back pain, with up to 20 per cent of those undergoing surgery at some point to relieve the nagging discomfort.
Many of those procedures are done with a minimally invasive approach rather than open surgery, thereby reducing both the time to perform surgery and the trauma experienced by the patient. Sometimes, however, the area of the spinal cord or nerve root compression can be obscured by body parts, which can result in ongoing symptoms or the need for further surgery.
Dalhousie researchers think they can change that by giving surgeons ‘eyes’ on the injury.
They have developed a sleek, high-resolution probe that can travel to the site of the spinal compression and provide a clear view of the surgical area before and after the procedure is done to make sure the nerve has been decompressed.
The result? A significant reduction in the number of surgeries that have to be repeated.
“It goes right next to the spinal cord in the surgical pathway,” says Dr. Jeremy Brown, a professor in Dalhousie’s School of Biomedical Engineering, who developed the endoscopic imaging probe. “So, you can take some images before the surgeon removes the herniated disc or whatever is compressing the spinal cord, the surgeon then removes the material surgically and then you take some more images and say, ‘OK, is the nerve still being compressed or is it free now?'”
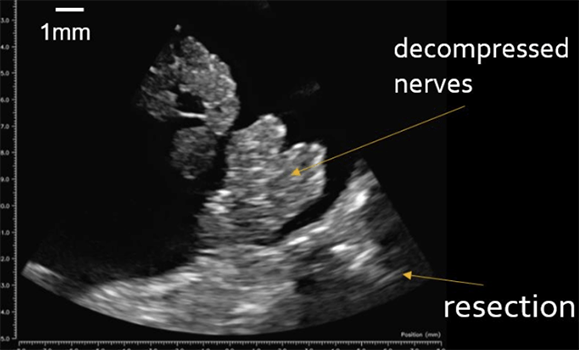
High-resolution image captured by researchers shows a decompressed nerve.
A vivid view previously unseen
The probe is guided to the site of the compression through 18-millimetre tubes and can then begin to capture images. After receiving Research Ethics Board approvals to use the device on 20 patients, Dr. Brown worked with Dalhousie professor and neurosurgeon, Dr. Sean Christie, to test the probe on an observational basis and validate its efficacy.
So far, Dr. Brown has used the probe on three patients undergoing spinal cord surgeries. The results were remarkable, with the probe providing a vivid view of the spinal anatomy and nerves previously unseen by the surgeon.
“What was surprising was because the resolution is amazingly high, we saw anatomy inside of the sac that goes around spinal cord. We could see nerves and other things that the surgeon said we had never seen before,” says Dr. Brown, adding that this raised the possibility of using the probe in other medical procedures.
“It made us wonder how we can maximize the patient outcomes with this tool — the image quality is really great!”

Dr. Sean Christie threads the imaging probe down a tube. (Jeremny Brown image)
Changing approaches to surgery
Dr. Christie also sees direct benefits to this technology.
“It has always been a challenge to verify intraoperatively that there isn’t a small fragment of disc that is just out of your field of view which could still be causing a problem. Currently, we need to gently manipulate the nerve or blindly palpate beneath it to confirm adequate decompression,” he says.
 “With this new probe, we can now clearly see the decompressed nerve floating freely in the spinal fluid! This will change our approach to spinal surgery and open the door for even more minimally invasive procedures.”
“With this new probe, we can now clearly see the decompressed nerve floating freely in the spinal fluid! This will change our approach to spinal surgery and open the door for even more minimally invasive procedures.”
Roughly 1.5 million spine surgeries are done in the United States every year. More locally, Nova Scotia Health does about 900 of the procedures a year. Of those, it’s thought that 30 to 40 per cent use minimally invasive approaches that result in less blood loss and trauma for the patient.
The remaining 25 to 30 per cent are done through more invasive open surgeries, something Dr. Brown believes could be further reduced with the use of the imaging tool.
It’s hoped that after 20 patients he and his team will be able to demonstrate that they can visualize, for example, a nerve being decompressed or a residual tumour being present in the brain and then receive approvals to allow a surgeon to operate based on the imaging.
Other applications
It’s also possible the ground-breaking technology could be used in about 20 other surgeries that are mostly done in a minimally invasive manner, such as those to treat aneurysms, brain tumours and pituitary tumours.
Dr. Brown, who has been working on the probe for about 10 years, originally designed the 3mm-by-3mm device to treat cancerous brain tumours. The innovation offered up an opportunity that pushed the boundaries of brain cancer treatment with an ultrafast imaging platform that allows surgeons to see brain tumours with five to 10 times the resolution of conventional imaging.
In that procedure, the device is inserted through a small keyhole created in the skull and allows surgeons to follow an exact path to the tumour so that it can be surgically removed. While the probe itself is already a first of its kind, Dr. Brown is now working on a secondary feature for it — a therapeutic tool that will non-invasively vaporize cancerous tissues with high-intensity sound waves.

Dr. Jeremy Brown and operating room staff view images produced by the probe on a monitor. (Provided photo)

