Princeton University will open COVID-19 testing laboratory for campus community
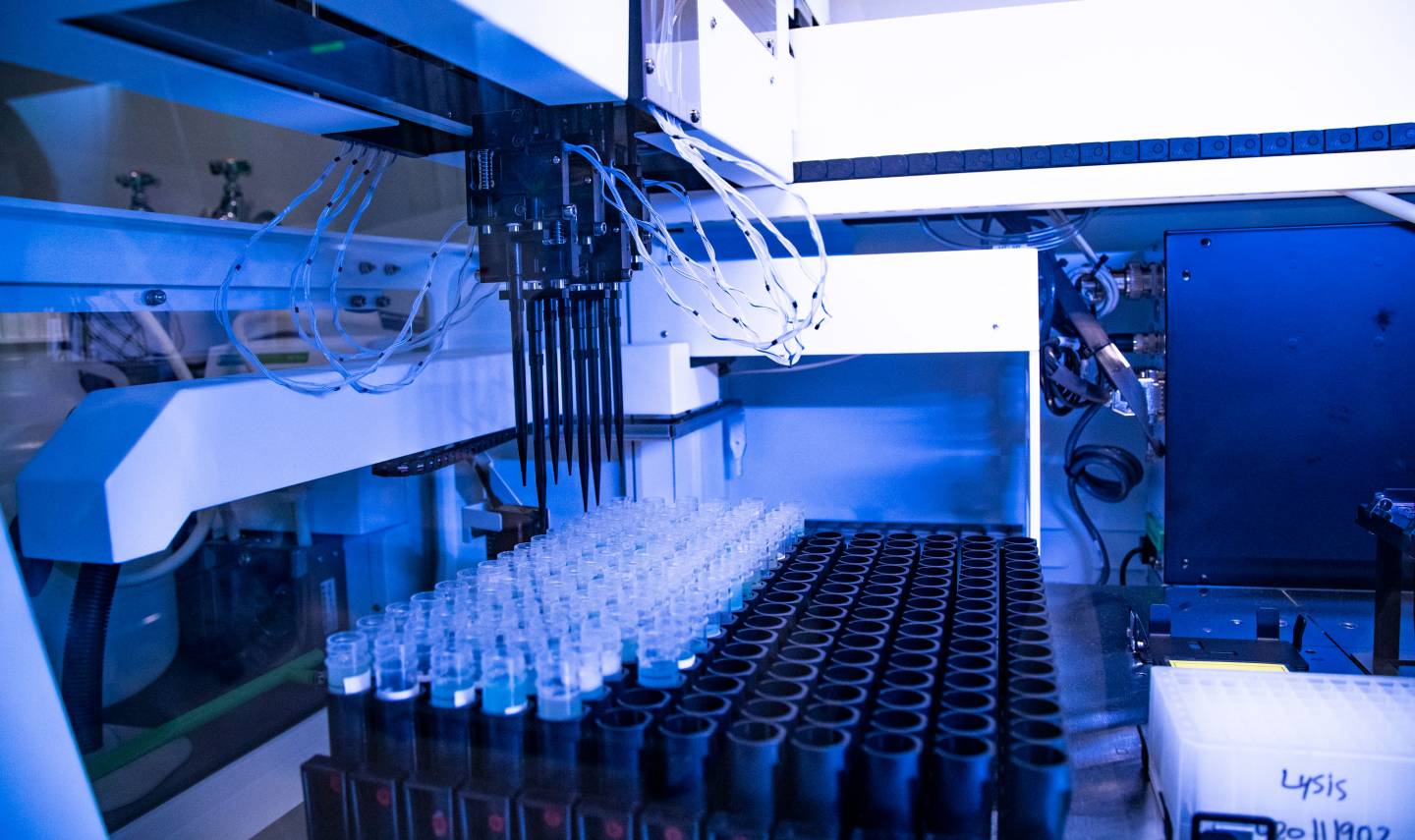
Princeton University is opening a new COVID-19 testing laboratory to support its comprehensive testing program for students, faculty, staff and researchers approved to be on campus. The in-house clinical laboratory will facilitate increased testing capabilities with faster results. The lab’s opening is an important step as the University considers how to safely increase density on campus and support the return of residential education.
Princeton is one of only a few universities in the country without a medical or veterinary school to build a federally certified COVID-19 testing lab.
“As the dire nature of the pandemic became clear last spring, President [Christopher L.] Eisgruber made the bold decision that the University would build and seek a license for its own testing laboratory,” said Daniel Notterman, a physician and University lecturer with the rank of professor in the Department of Molecular Biology. “At the time, resources and testing capabilities were extraordinarily scarce, and he was determined that the University, as it worked to reopen the campus, would contribute to the testing capacity in New Jersey by creating resources to test its own students, faculty, staff and researchers.”
Notterman added: “The leadership of the University very early realized that if we were to have any semblance of a normal community, with people repopulating and enlivening our campus, we would need to have a testing program. Princeton stood this lab up in six months — that’s remarkable. It makes me proud of the University.”
Paul LaMarche, vice provost for space programming and planning, said creating the lab was an all-hands-on-deck effort.
“The University worked really, really hard getting this done,” LaMarche said. “A lot of people dropped what they were doing to come to our aid to make this a successful enterprise. We got a tremendous amount of support and help from the University community pitching in to get this going, from procurement to facilities to faculty and staff. In addition, a group of administrators, faculty and staff led by Ramona Romero [vice president and general counsel] met frequently to guide and lend vital support to these efforts.”
An intense process involved construction, permitting, purchasing equipment, designing a data system, hiring and training skilled staff, and obtaining the required governmental approvals. The University’s lab was certified under the federal Clinical Laboratory Improvement Amendments (CLIA) on September 3, and was licensed by the New Jersey Department of Health’s Division of Public Health and Environmental Laboratories, effective Nov. 6. CLIA certification means the University may test samples for COVID-19 and distribute the results of such tests to the individuals tested.
Bonnie Bassler chairs the Department of Molecular Biology, where the lab is housed. She said: “From nothing, from not even a gleam in anybody’s eye, to a few months later having this state-of-the-art, high capacity, functioning and accredited site — that kind of grit and determination and commitment from a lot of players, I think, speaks to Princeton’s character.”
While the new testing laboratory is not a research laboratory, it reflects Princeton’s standing as a leading research institution.
“Our research mission is about solving urgent biomedical problems, so there’s an incredible match between this unique need and our mission,” said Bassler, the Squibb Professor in Molecular Biology.
The lab is designed to run at least 2,000 individual samples per day, or 10,000 per work week. The University plans to explore the possibility of increasing capacity by pooling samples — in other words, testing a certain number of samples as a group. If the group tests negative, all the specimens are known to be negative. If the combined sample tests positive, the specimens are then individually re-tested.
“The goal is to identify positive cases early enough — before people have been able to spread the virus to others — so as to isolate the cases as soon as possible and stop community spread and prevent outbreaks or clusters,” said Irini Daskalaki, an infectious disease physician at University Health Services (UHS). “We depend on regular testing to catch people early, in the presymptomatic or asymptomatic stage, because actually that’s when they are most infectious.”
Testing, contact tracing and patient privacy
The testing method the University is using is very sensitive. It uses a qPCR (a quantitative polymerase chain reaction) that multiplies the amount of SARS-CoV-2 genetic material in each sample, so even very early infections are detectable.
The test looks for three SARS-CoV-2 genes; when none is detected, the test is negative. When only one of the three tested genes is detectable, the person sampled will be told that their test was indeterminate, and they will need to submit another sample. If two or three genes show detectable levels, the test is labeled positive.
The lab uses saliva samples instead of a nasal swab, which the University’s medical staff recommended for several reasons. The saliva test is as accurate as the deep nasal swab, and more accurate than the shallower self-swabbing common at drive-through testing sites. The saliva sample can also be self-collected, thereby protecting healthcare providers and reducing the need for personal protective equipment.
“It’s also much more comfortable than the nasal pharyngeal swab, the deep swab. We didn’t want to subject students to something uncomfortable on a regular basis,” said Notterman.
Notterman, a pediatrician, said his concern for the comfort and safety of the greater Princeton community is paramount. “I’m very motivated, not only to help protect my students and my colleagues and staff at the University, but also to work with all of the wonderful people here to help protect the larger community by keeping the level of infection at the University as low as possible.”
Each saliva sample tube is identified by a barcode that is scanned into the app before the sample collection. The barcodes are then scanned by the testing machines in the lab at every stage of the multi-step testing, so every sample’s journey is fully documented while protecting patient privacy.
Once the testing is complete, the barcode-identified results are transmitted to UHS staff, who will match the barcode with each person’s name and let people know their results.
“Our team’s approach throughout the fall has been to check hourly for new results and to call those who test positive,” said Daskalaki, who serves as UHS’s Global and Community Health physician. “Whenever possible, we want people to learn of their positive results from a member of the UHS team, not an email or an app. We understand that usually this is a surprise for them, so we really want to be there for them and be able to answer their questions. We provide information about isolation, what to expect in the coming days, how we’re going to support and follow up with them, and that their contacts are going to be notified by us.”
Daskalaki said that as soon as a UHS physician gives the results, a Global and Community Health team member starts the contact tracing process. “People who test positive don’t need to notify their contacts. We do that on their behalf and without revealing their identity.”
McCosh Health Center to continue to test students experiencing symptoms
The University will continue to provide testing to students who are experiencing symptoms at McCosh Health Center. Employees who are experiencing symptoms may receive testing through their personal physician, urgent care centers, county health resources or the University’s VitalCheck virtual health program.
For students with a fever, cough or other COVID-19 symptoms, McCosh medical personnel will provide 45-minute “rapid PCR tests.” These may require a higher level of viral load to show a positive test, but people with enough SARS-CoV-2 particles to have manifested symptoms of COVID-19 are likely to have enough of a viral load to be easily detected by the rapid system.
“When a patient presents with respiratory symptoms, we will be able to test and provide them with results right then and there,” said Daskalaki. “Especially as we’re entering flu season, it’s very important to be able to differentiate whether a student with flu-like symptoms has COVID or not, because if we don’t know, then we’ll have to assume they do, and they would need to be isolated until their results are back.”
Testing is an integral part of overall health and safety measures
The opening of the CLIA-certified lab is part of the University’s ongoing efforts to promote health and safety on campus. As Daskalaki and other medical professionals note, testing is most effective when coupled with other risk-reducing behaviors such as mask wearing, social distancing, staying away from others if feeling ill and washing hands frequently.
“We are extraordinarily proud of our new CLIA-certified lab,” said Daskalaki, “as it provides one important component of the University’s many efforts to help keep our students, faculty and staff safe.”