Cardiovascular Health Of Offspring Remains Safe From Fertility Treatment- Study
The University of Bristol-led study, published in European Heart Journal today [6 February 2023] sought to address concerns around whether fertility treatment leads to adverse cardiometabolic health in offspring. The data sample included 8,600 children from Bristol’s Children of the 90s study, a world-leading health study which has followed pregnant women and their offspring since 1991.
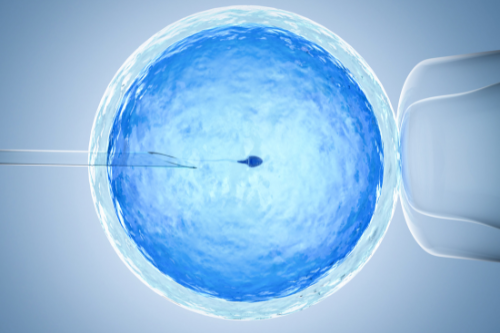
Since the first birth of a child by in vitro fertilisation (IVF), questions have been raised about the health risks to children conceived this way, however previous studies are limited by small sample size, short follow-up, and unsatisfactory comparison groups.
The study, led by an international research group from the Assisted Reproductive Technology and Health (A.R.T-Health) Partnership, looked at data from 35,000 European, Singaporean, and Australian offspring. It was large enough to study whether conception by ART affected blood pressure, pulse rate, lipids or glucose from childhood to young adulthood (up to early 20s).
The researchers found that blood pressure, heart rate, and glucose levels were similar in children conceived using ART and their naturally conceived peers. The team also found that those who were conceived by ART had slightly higher cholesterol levels in childhood, which did not persist to adulthood, and some indication of slightly higher blood pressure in adulthood.
Dr Ahmed Elhakeem, Research Fellow in Epidemiology in Bristol Medical School: Population Health Sciences (PHS) at the University of Bristol, and lead study author, said: “This is the largest study of its kind, and could not be conducted without data from studies such as Children of the 90s. Parents conceiving or hoping to conceive through assisted reproductive technology and their offspring should be reassured that cardiometabolic health appears to be comparable in ART-conceived and naturally conceived children. Studies with longer follow-up would now be beneficial to examine how results might change across adulthood.”
Deborah Lawlor, Professor of Epidemiology, MRC Investigator and British Heart Foundation Chair and senior author from Bristol Medical School: PHS, added: “This important research is only possible through large scale international collaboration and longitudinal health studies, where participants contribute health data throughout their entire lives. We are particularly grateful to the European Research Council, British Heart Foundation and UK National Institute for Health Research for making this possible and to all of the study participants and researchers.”
Peter Thompson, Chief Executive, The Human Fertilisation and Embryology Authority (HFEA), said: “Each year around 60,000 patients use fertility services in the UK in the hope of one day having a family of their own. Those patients should be reassured by this study which shows that the heart health of children born from assisted reproduction technologies, like IVF, are no different from children conceived naturally.
“Science and research move rapidly in the fertility sector but it is widely acknowledged that more large scale studies like this are needed to continually drive improvements in care. Health outcomes in children conceived using assisted reproductive technologies are a high priority for the HFEA and we monitor the latest research and provide information for patients and professionals. Anyone considering fertility treatment in the UK should visit www.hfea.gov.uk for high quality impartial information on treatment options and licensed clinics.”
The study was funded by the European Research Council under the European Union’s Horizon 2020 research and innovation program, Medical Research Council (MRC), British Heart Foundation (BHF) and National Institute for Health and Care Research Bristol Biomedical Research Centre (NIHR Bristol BRC).