Charité Study Shows Triple Combination Therapy Dramatically Improves Lung Function in Children with Cystic Fibrosis
Cystic fibrosis is a hereditary disease that so far has been incurable. Those affected have thick, viscous mucus secretions in their lungs, and lung function diminishes steadily over time. Today, triple combination therapy makes it possible to address the root causes of the defect underlying the disease. This form of treatment was recently approved for children in addition to adults. A recent observational study led by Charité – Universitätsmedizin Berlin shows that the new treatment significantly improves the health status of school-aged children with cystic fibrosis. The results have been published in the European Respiratory Journal.*
People with cystic fibrosis experience a buildup of thick, viscous mucus secretions in the lungs, clogging their airways. This leads to shortness of breath, chronic bacterial infections, inflammation and tissue changes in the lungs, with diminishing lung function. Lifelong symptomatic treatment involving daily inhalation of mucus-thinning medications, antibiotics in certain cases, and physical therapy is recommended for those with the disease.
A new therapeutic concept emerged in 2020 as a way to address not only the symptoms, but the cause of the disease: combination therapy with three drugs called elexacaftor, tezacaftor, and ivacaftor. This “triple combination therapy” is taken as a pill and was approved for children six years and older in 2022 and then, in 2023, starting at the age of two years.
“Having this therapy become available for children is a real blessing for our young patients,” says Prof. Mirjam Stahl, corresponding author of the study and head of the Division of Cystic Fibrosis at the Department of Pediatric Respiratory Medicine, Immunology and Critical Care Medicine at Charité. “In our recent observational study, which we conducted on children ranging in age from six to eleven years, we were able to show that triple combination therapy leads to a significant improvement in the lung disease.”
How the triple combination therapy works
As a disease, cystic fibrosis is based on genetic defects that cause the molecular structures responsible for normal production of mucus that covers the airway surfaces of the lungs, known as CFTR channels, to work inadequately or not at all. CFTR channels regulate the transportation of salt and water across airway surfaces ensure that the mucus formed is liquid enough. About 90 percent of cystic fibrosis patients have a mutation known as F508del, which causes structural damage to the CFTR channel, so it is not functional.
Two of the drugs involved in the triple combination therapy, elexacaftor and tezacaftor, can correct this structural damage. The third one, ivacaftor, acts as a kind of wedge, keeping the CFTR channel open at all times. “Triple combination therapy makes it possible to boost the functioning of the CFTR channel to as much as 50 percent of normal levels,” Stahl says. “We know from a previous observational study of adults that the triple combination therapy is associated with considerable improvement in lung function and quality of life. It’s a true game changer for the majority of patients.”
Lung function comparable to healthy subjects
But how effective is the triple combination therapy in children of elementary school age? The team of researchers led by Stahl and Prof. Marcus Mall, Director of the Department of Pediatric Respiratory Medicine, Immunology and Critical Care Medicine and the head of the observational study, aimed to find out. The study was conducted at four German cystic fibrosis centers. In addition to Charité, the Hannover Medical School (MHH), Heidelberg University Hospital, and the University Hospital of Giessen were also involved.
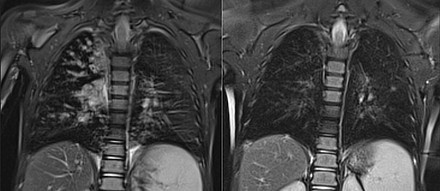
The researchers studied 107 children with cystic fibrosis ranging in age from six to eleven years, both before the treatment started and during the prescribed triple combination therapy. Typical examination methods for gauging lung function, such as spirometry, were paired with new and innovative methods such as multiple breath washout and magnetic resonance imaging (MRI) of the lungs. These methods made it possible to detect and visualize changes in the lungs such as widening of the bronchi, thickening of the bronchial walls, and persistent mucus deposits in great detail.
The team of researchers followed the study participants for about a year. “Triple combination therapy significantly reduced the severity of lung disease in young patients and, at least during the one-year study period, also prevented the disease from progressing,” Mall says, summarizing the results of the study. “The majority of the children even achieved normal lung function with the triple combination therapy. That’s a highly positive result!”