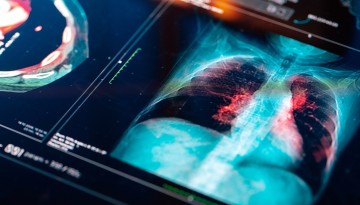
Genetic Signature Offers Potential to Predict Lung Cancer Response to Immunotherapy
A new study has identified a set of 140 genes that may help predict enhanced disease-free survival in patients with non-small-cell lung cancer (NSCLC) treated with a combination of immunotherapy and low-dose radiation.
The results, published Feb. 23 in Cell Medicine Reports, suggested that this “gene signature” could be used to identify a subclass of lung tumors that is more likely to be eradicated by immunotherapies.
Corresponding authors of this study were Dr. Nasser Altorki, the David B. Skinner, M.D. Professor of Thoracic Surgery at Weill Cornell Medicine; and Timothy McGraw, professor of biochemistry at Weill Cornell Medicine.
Immunotherapy – which activates a person’s own immune system to attack cancer – has saved countless lives, but only 20% to 25% of patients respond to it. Predicting who would benefit from this approach, and why, could help patients who have exhausted other options, such as chemotherapy.
Studying a cohort of 60 patients with NSCLC, the team previously determined that adding a low dose of radiation to a course of durvalumab, an immune-boosting drug, promoted cancer-free survival in most of these individuals. Now, to assess why some tumors didn’t respond to the therapy, the researchers examined pretreatment tumor biopsies from this study cohort. They determined the gene expression profiles, which showed the specific genes that are turned up and those that turned down in each sample.
They compared the gene expression profiles of 10 tumors that reached major pathologic response (MPR) – the elimination of more than 90% of the cancer cells in patients’ tumors – with combination treatment, versus six that did not. They discovered the two groups of pretreatment tumors could be reliably distinguished by a set of genes with 135 of the genes turned up and five turned down. The majority of the 135 genes were associated with enhanced cell growth, suggesting the tumors that responded to the dual therapy were particularly aggressive.
The researchers were also able to examine how the gene expression profile changed in the responsive cancers before and after treatment. They found that in tumors displaying MPR, dual therapy not only reversed the activity of this 140-gene set, it also increased the activation of genes associated with cellular pathways involved in immunity and tissue repair.
The activity of the 140 genes which correlated with treatment response is particularly promising as clinicians could use the signature to identify people who would gain the maximum benefit from immunotherapy.
The researchers plan to test whether tumors with this aggressive gene signature have a better response to the combination therapy in a larger patient study.
Also contributing was Olivier Elemento, professor of computational genomics at Weill Cornell Medicine and director of the Englander Institute for Precision Medicine.