International Team Discovers Boosting Key Protein in Eye Cells Could Prevent Age-Related Vision Loss
Progression of age-related macular degeneration (AMD) — a common condition impacting central vision, for which there are currently no effective treatments, affects around 200-million people worldwide. This number is expected to rise to 288-million by 2040 as the population ages. This new breakthrough could lead to new and more effective AMD treatments.
AMD can severely impact a person’s vision. Patients suffering from AMD often start with blurred vision or seeing a black dot in their central vision, which can ultimately expand to the point where there is no useful central vision. The exact cause of AMD is complex and thought to involve a combination of aging, genetics, environment and lifestyle factors.
Primarily affecting people over the age of 50, the risk of developing AMD significantly increases with age and makes tasks like reading and driving difficult.
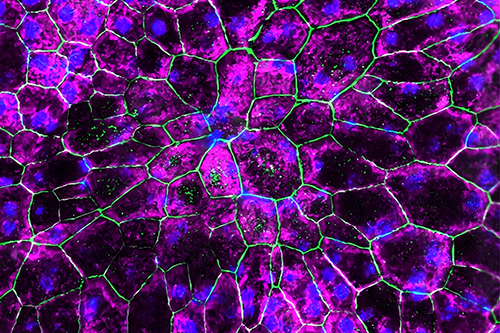
Scientists believe that chronic inflammation, which is typical with aging, is associated with the reduction of a key immune regulatory protein called IRAK-M. This protein is crucial for protecting the retinal pigment epithelium (RPE), a layer of cells essential for maintaining a healthy retina. When RPE cells are damaged, it can result in serious eye conditions and vision loss.
In this study, researchers investigated the role of IRAK-M in AMD by examining genetic variations and their link to AMD risk. By studying IRAK-M levels in patient samples and mouse models of retinal degeneration, the team observed changes in retinal function in mice lacking the IRAK3 gene, which expresses the IRAK-M protein. They found that IRAK-M decreases with age, especially in the retinal pigment epithelium (RPE), and this decline is more pronounced in those with age-related macular degeneration (AMD).
The team then sought to explore whether increasing IRAK-M could protect retinal cells from degeneration in mouse models and whether it is a potential therapeutic target for macular degeneration. They show that increasing IRAK-M levels through RPE-specific gene delivery helps protect against the effects of aging and oxidative stress and reduces retinal degeneration.
Andrew Dick, Professor of Ophthalmology from Bristol Medical School at the University of Bristol, Director of the UCL Institute of Ophthalmology and one of the study’s lead authors, says: “Our findings suggest that boosting a protein called IRAK-M could be a potential treatment strategy for AMD and could offer an exciting new therapeutic target for this common condition for which effective therapies remain elusive.”
Dr Jian Liu, the lead author and senior research scientist at the Academic Unit of Ophthalmology at the University of Bristol, adds: “Since age stands as the primary risk factor for AMD, the gradual decrease of IRAK-M levels with age and a further decline in AMD signifies intricate biological mechanisms underlying the disease’s development and suggests a potential marker of early AMD progression.”
The authors aim to help develop the therapies further through a new University of Bristol spin-out company called Cirrus Therapeutics.
Dr Ying Kai Chan, Cirrus Therapeutics co-founder and Chief Executive Officer, and one of the study’s co-lead authors, says: “This discovery will build and improve upon current treatments for AMD, which are targeting single pathophysiology pathways. Our novel approach not only addresses the multiple pathways involved in treating AMD but also offers the most compelling and evidence-based strategy available today.”
The research was funded by the Rosetrees Trust; Stoneygate Trust; Underwood Trust; Macular Society; Sight Research UK; Moran Eye Center and Sharon Eccles Steele Center for Translational Medicine (SCTM) at the University of Utah, USA, and supported by the National Institute for Health and Care Research (NIHR) BRC Moorfields and UCL-Institute of Ophthalmology.