Researchers Develop Grafts that Replicate the Human Ear
Using state-of-the-art tissue engineering techniques and a 3D printer, researchers at Weill Cornell Medicine and Cornell Engineering have assembled a replica of an adult human ear that looks and feels natural.
The study, published March 16 in Acta Biomaterialia, offers the promise of grafts with well-defined anatomy and the correct biomechanical properties for those who are born with a congenital malformation or who lose an ear later in life.
“Ear reconstruction requires multiple surgeries and an incredible amount of artistry and finesse,” said senior author Dr. Jason Spector ’91, chief of the Division of Plastic and Reconstructive Surgery at NewYork-Presbyterian/Weill Cornell Medical Center and a professor of surgery (plastic surgery) at Weill Cornell Medicine. “This new technology may eventually provide an option that feels real for thousands needing surgery to correct outer-ear deformities.”
Spector worked on this project with long-time collaborator Larry Bonassar, the Daljit S. and Elaine Sarkaria Professor in Biomedical Engineering in the Meinig School of Biomedical Engineering, at Cornell Engineering.
Many surgeons build a replacement ear using cartilage removed from a child’s ribs, an operation that can be painful and scarring. And though the resulting graft can be crafted to resemble the recipient’s other ear, it generally does not have the same flexibility.
One way to produce a more natural replacement ear is to enlist the aid of chondrocytes, the cells that build cartilage. In earlier studies, Spector and his colleagues used animal-derived chondrocytes to seed a scaffold made of collagen, a key component of cartilage. Though these grafts developed successfully at first, over time the well-defined topography of the ear – its familiar ridges, curves and whorls – were lost.
“Because the cells tug on the woven matrix of proteins as they labor, the ear contracted and shrank by half,” Spector said.
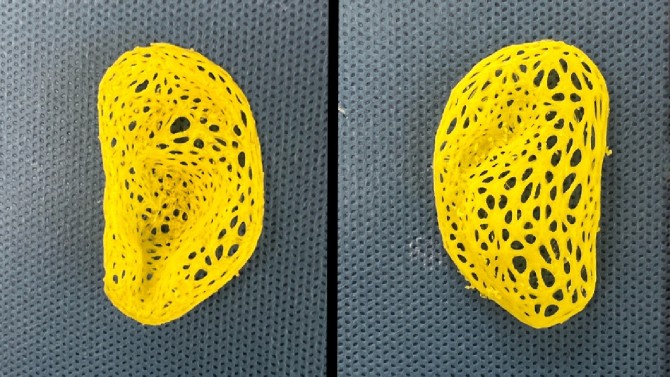
To address this problem in this study, Spector and his team used sterilized animal-derived cartilage treated to remove anything that could trigger immune rejection. This was loaded into intricate, ear-shaped plastic scaffolds that were created on a 3D printer, based on data from a person’s ear. The small pieces of cartilage act as internal reinforcements to induce new tissue formation within the scaffold. Much like rebar, it strengthens the graft and prevents contraction.
Over the next three to six months, the structure developed into cartilage-containing tissue that closely replicated the ear’s anatomical features, including the helical rim, the “anti-helix” rim-inside-the-rim and the central, conchal bowl.
“That’s something that we had not achieved before,” Spector said.
Spector and Bonassar conducted biomechanical studies to test the feel of the ear. This confirmed that the replicas had flexibility and elasticity similar to human ear cartilage. However, the engineered material was not as strong as natural cartilage and could tear.
To remedy this issue, Spector plans to add chondrocytes to the mix, ideally ones derived from a small piece of cartilage removed from the recipient’s other ear. Those cells would lay down the elastic proteins that make ear cartilage so robust, producing a graft that would be biomechanically much more similar to the native ear, he said.
This work was supported in part by a grant from the National Institutes of Health.