Study Finds Waist-to-Height Ratio Detects Fat Obesity in Children and Adolescents Significantly Better than BMI
The study is the largest and the longest follow-up dual-energy x-ray absorptiometry (DEXA)-measured fat mass and muscle mass study in the world using Bristol’s Children of the 90s data (also known as the Avon Longitudinal Study of Parents and Children).
The prevalence of childhood and adolescent obesity has reached an epidemic proportion and is affecting nearly one in four children in the current decade. Unfortunately, obesity in the young population has been associated with cardiovascular, metabolic, neurological, musculoskeletal diseases and premature death in adulthood. Accurately detecting overweight and obesity in children is critical to initiating timely interventions.
For nearly a generation, weight-to-height ratio charts and BMI for age and sex have been used to diagnose children with obesity. However, these assessment tools are inaccurate in childhood and adolescence since they do not distinguish fat mass from muscle mass.For instance, two children with similar BMI might have different proportions of fat and muscle mass which makes obesity diagnosis difficult.
Expensive tools such as the DEXA scan accurately measures fat and muscle content of the body, but this device is not readily available in primary health care centres. Recently, the American Academy of Pediatrics (AAP) published a clinical guideline on childhood obesity and requested urgent research on inexpensive and accurate alternative measures of obesity.
Emerging studies in adults appear to suggest that waist circumference-to-height ratio predicts premature death better than BMI and could be a potential added tool to BMI measure in improving the diagnosis of obesity.
However, there has been no former evaluation of how much waist circumference-to-height ratio measurements agree with DEXA-measured fat mass and muscle mass during growth from childhood to young adulthood. In addition, the threshold of waist circumference-to-height ratio needed to detect excess fat in children is not clear, which is why this study was carried out.
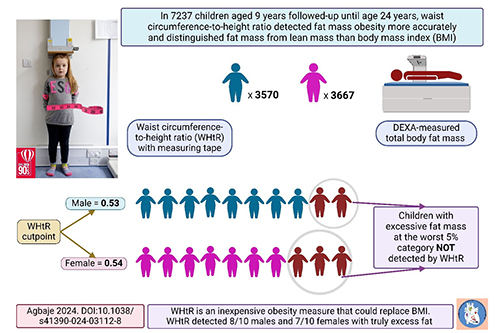
The research included 7,237 children (51 per cent females) aged nine years who were followed-up until age 24 years from Children of the 90s data. Their BMI and waist circumference-to-height ratio were measured at ages 9, 11, 15, 17, and 24 years. When different devices measure a variable with an exact resemblance, it is described as perfect agreement of the devices with a score of 100 per cent. For example, two DEXA scans from different manufacturers would measure fat mass with a near-perfect agreement of 99 to 100 per cent.
Waist circumference-to-height ratio had a very high agreement of 81 – 89 per cent with DEXA-measured total body fat mass and trunk fat mass, but a low agreement with muscle mass (24 – 39 per cent). BMI had a slightly high agreement with total fat mass and trunk fat mass (65 – 72 per cent) and muscle mass (52 – 0.58 per cent). Since BMI had a slightly high agreement with DEXA-measured muscle mass, it is difficult to specify whether BMI measures excess fat or muscle mass.
The optimal waist circumference-to-height ratio cut points that predicted the 95th percentile of total fat mass in males was 0.53 and 0.54 in females.This cut point detected eight out of ten males and seven out of ten females who truly had excess DEXA-measured fat. The cut point also identified 93 out of 100 males and 95 out of 100 females who truly do not have excess fat.
Professor Andrew Agbaje, Physician and Pediatric Clinical Epidemiologist at the University of Eastern Finland, said: “This study provides novel information that would be useful in updating future childhood obesity guidelines and policy statements. The average waist circumference-to-height ratio in childhood, adolescence, and young adulthood is 0.45, it does not vary with age and among individuals like BMI.
“Waist circumference-to-height ratio might be preferable to BMI assessment in children and adolescent clinics as an inexpensive tool for detecting excess fat. Parents should not be discouraged by the BMI or weight of their children but can inexpensively confirm whether the weight is due to increase in excess fat by examining their child’s waist circumference-to-height ratio.”
Julian Hamilton-Shield, Professor in Diabetes and Metabolic Endocrinology in the Bristol Medical School: Translational Health Science (THS), commenting on the study, added: “This present study from Dr Agbaje confirms the continued value of the Children of the 90s longitudinal cohort, whilst strengthening the evidence for waist-height ratio being a key measure of adiposity. Examining the same cohort, we believe this simple measure adds value in identifying those most at risk of obesity related liver disease across the life-course.”